Pterygium
Pterygium (surfer’s eye) is a very common condition amongst Australians.
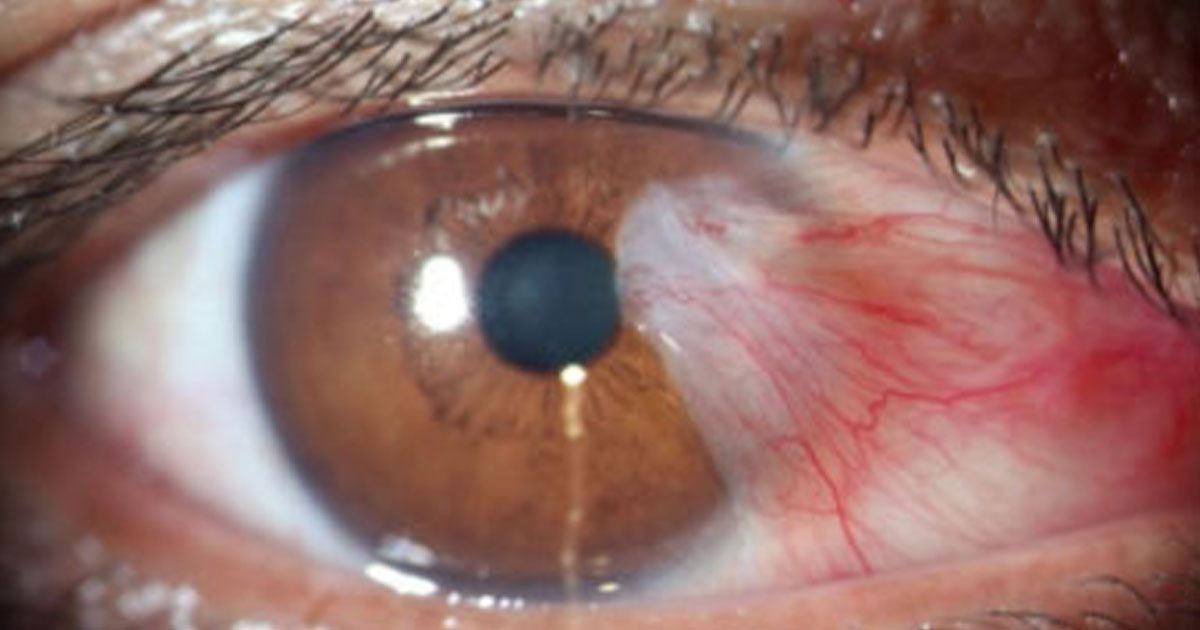
It is a fleshy triangular growth of the conjunctiva that overlaps the cornea, usually on the nasal side of the eye.
What causes pterygium?
Pterygia are caused by long-term exposure to UV light, as well as low humidity and dust. It is therefore a common finding in Australians who spend a lot of time outdoors.
What are the symptoms of pterygium?
Pterygia can become intermittently irritated and inflamed, causing tearing, foreign-body sensation, and ocular surface discomfort.
Advanced pterygia can cause distortion of the corneal shape, resulting in astigmatism. Once encroached on the visual axis, they can cause reduction in visual acuity.
What are the treatment options for pterygium?
Conservative management involves the use of lubricating eye drops for symptom relief. Topical steroid drops should be used very sparingly for inflamed pterygia due to their side effects of glaucoma and cataract formation.
The definitive treatment of pterygium is surgical, and involves excision of the pterygium, and placement of a conjunctival autograft in its place to prevent recurrence (as shown in pictures d and e below):
It is a fleshy triangular growth of the conjunctiva that overlaps the cornea, usually on the nasal side of the eye.
What causes pterygium?
Pterygia are caused by long-term exposure to UV light, as well as low humidity and dust. It is therefore a common finding in Australians who spend a lot of time outdoors.
What are the symptoms of pterygium?
Pterygia can become intermittently irritated and inflamed, causing tearing, foreign-body sensation, and ocular surface discomfort.
Advanced pterygia can cause distortion of the corneal shape, resulting in astigmatism. Once encroached on the visual axis, they can cause reduction in visual acuity.
What are the treatment options for pterygium?
Conservative management involves the use of lubricating eye drops for symptom relief. Topical steroid drops should be used very sparingly for inflamed pterygia due to their side effects of glaucoma and cataract formation.
The definitive treatment of pterygium is surgical, and involves excision of the pterygium, and placement of a conjunctival autograft in its place to prevent recurrence (as shown in pictures d and e below):
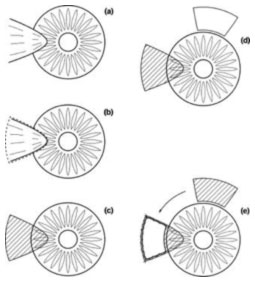
The conjunctival graft can either be sutured in place, or secured with fibrin glue. The latter is Dr Robaei’s preferred technique because it offers better post-operative recovery and comfort, as well as reduced recurrence risk.
It is important to note that up to 10% of pterygia harbour areas of squamous dysplasia, with potential for malignant transformation. Any recent change in the size or appearance of a pterygium should prompt referral to an ophthalmologist for expert assessment.
It is important to note that up to 10% of pterygia harbour areas of squamous dysplasia, with potential for malignant transformation. Any recent change in the size or appearance of a pterygium should prompt referral to an ophthalmologist for expert assessment.
