
Viral Conjunctivitis - What is it and how is it treated?
Viral conjunctivitis is a self-limiting condition, and the commonest cause of a red eye presentation in general practice. It is typically caused by adenovirus. Other, less common viruses include herpes simplex, herpes zoster, enterovirus, and coxsackie virus.
Viral conjunctivitis is highly contagious. The incubation period is usually 7-10 days, and the period of contagion typically lasts 10-12 days. Transmission occurs by contact with infected tears or upper respiratory droplets.
Unlike bacterial conjunctivitis, which is far less common, viral conjunctivitis runs a protracted course, with worsening of symptoms over the first week, followed by slow resolution over 3-4 weeks.
Typical symptoms include:
Diagnosis of viral conjunctivitis is usually clinical, although a viral swab for adenovirus PCR can be used to confirm the diagnosis.
Clues which help the GP differentiate viral conjunctivitis from other less common, and potentially more serious causes of a red eye include:
1. Presence of eyelid oedema. This is a universal finding, which is typically absent in other causes of red eye, including those caused by bacterial conjunctivitis, allergic eye disease, iritis, or corneal infection.
2. Presence of tender pre-auricular adenopathy
3. A red eye that is initially unilateral, and subsequently affects the second eye within days
4. Recent history of contact with persons with viral conjunctivitis
5. Absence of other red flag features, such as contact lens wear, reduced vision, or photophobia.
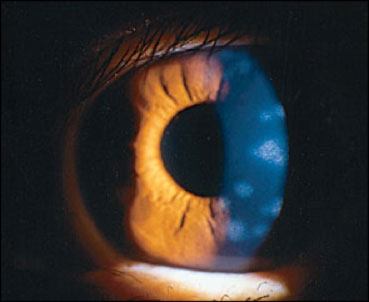
Ten percent of patients with adenoviral conjunctivitis go on to develop corneal involvement towards the end of week 2. This is an immune keratitis with white deposits in the cornea, causing significant reduction in vision, as well as prominent photophobia. This, ‘nummular keratitis’ requires treatment with a weak topical steroid such as fluorometholone (FML), and therefore requires referral to an ophthalmologist.
Viral conjunctivitis is highly contagious. The incubation period is usually 7-10 days, and the period of contagion typically lasts 10-12 days. Transmission occurs by contact with infected tears or upper respiratory droplets.
Unlike bacterial conjunctivitis, which is far less common, viral conjunctivitis runs a protracted course, with worsening of symptoms over the first week, followed by slow resolution over 3-4 weeks.
Typical symptoms include:
- Red eye, which most often begins unilaterally, and for this reason, often poses a diagnostic dilemma for the General Practitioner.
- Copious watery discharge, with absence of pus
- Matted eye lashes upon waking
- Ocular surface discomfort, but no frank pain
- Minimally blurred vision that clears with blinking
- Minimal to no photophobia
- Symptoms of a recent URTI
Diagnosis of viral conjunctivitis is usually clinical, although a viral swab for adenovirus PCR can be used to confirm the diagnosis.
Clues which help the GP differentiate viral conjunctivitis from other less common, and potentially more serious causes of a red eye include:
1. Presence of eyelid oedema. This is a universal finding, which is typically absent in other causes of red eye, including those caused by bacterial conjunctivitis, allergic eye disease, iritis, or corneal infection.
2. Presence of tender pre-auricular adenopathy
3. A red eye that is initially unilateral, and subsequently affects the second eye within days
4. Recent history of contact with persons with viral conjunctivitis
5. Absence of other red flag features, such as contact lens wear, reduced vision, or photophobia.
Ten percent of patients with adenoviral conjunctivitis go on to develop corneal involvement towards the end of week 2. This is an immune keratitis with white deposits in the cornea, causing significant reduction in vision, as well as prominent photophobia. This, ‘nummular keratitis’ requires treatment with a weak topical steroid such as fluorometholone (FML), and therefore requires referral to an ophthalmologist.
The treatment of viral conjunctivitis is entirely supportive. Cool compresses reduce eyelid oedema, and artificial tear drops improve comfort. Chloramphenicol has no role to play in viral conjunctivitis, and its preservative content can exacerbate ocular surface irritation.
Additionally, patients need to be counselled on the very contagious nature of their disease, the need for frequent hand washing, as well as minimising social activities to limit spread.
Additionally, patients need to be counselled on the very contagious nature of their disease, the need for frequent hand washing, as well as minimising social activities to limit spread.
